Total Cystectomy with Continent Urinary Diversion in Men
Total cystectomy is surgery to remove the bladder. It is most often done to treat bladder cancer. After the bladder is removed, a new bladder (neobladder) or a pouch is made inside the body to collect urine. This is called a continent urinary diversion. This procedure is different than incontinent urinary diversion, where urine drains constantly into a bag on the outside of the body.
Changes to your body
During simple cystectomy, the bladder is removed. During radical cystectomy, nearby lymph nodes and organs that the cancer may spread to are also removed. These may include some reproductive organs, such as the prostate and seminal vesicles. Removal of these organs can lead to problems with sexual function, including the ability to get or keep an erection. It may also lead to infertility. Your healthcare provider can tell you more about this and your options.
Types of urinary diversion
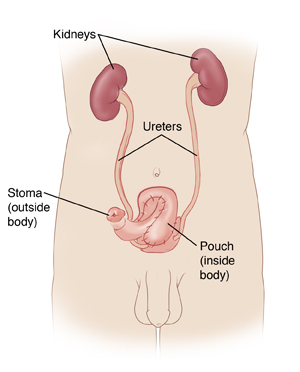
To collect urine inside your body, you may have a neobladder or a pouch. Your healthcare provider will discuss which option is best for you.
-
Neobladder. This allows urine to follow the normal path out of the body. A neobladder is made from a part of your small intestine that has been removed. With a neobladder, you’ll no longer have nerves that signal when your bladder is full. You will need to empty the bladder on a set schedule. To do this, you use your pelvic and belly (abdominal) muscles to help push the urine out of your body.
-
Pouch. This connects to the ureters on one end. The other end connects to a small, permanent opening (stoma) made in the belly wall. Most of the time, the stoma is covered with a small bandage. To empty urine from the pouch, you pass a catheter through the stoma into the pouch. This is done on a set schedule. Unlike with some treatments, no bag is needed to collect urine.
Getting ready for surgery
Prepare for the surgery as you have been told. In addition:
-
Tell your healthcare provider about all medicines you take. This includes prescription and over-the-counter medicines, vitamins, herbs, and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may need to stop taking some or all of them before surgery, as instructed by your provider.
-
Follow any directions you are given for not eating or drinking before your surgery. This includes coffee, water, gum, and mints. If you have been instructed to take medicines, take them with a small sip of water.
-
If you have been told to, prepare your bowel for surgery. This is called “bowel prep.” This process starts 1 to 2 days before the surgery. Your healthcare provider may tell you to limit your diet to clear liquids. You may also be asked to take laxatives or to give yourself an enema. Follow all instructions you are given.
The day of surgery
The surgery takes 4 to 6 hours. Afterward, you will stay in the hospital for 5 to 7 nights.
Before the surgery begins:
-
An IV (intravenous) line is put into a vein in your arm or hand. This delivers fluids and medicines, such as antibiotics. In some cases, a central or arterial line is inserted into a blood vessel somewhere else on the body. Your healthcare provider can tell you more.
-
You may get medicine to prevent blood clots in your veins.
-
To keep you free of pain during the surgery, you’re given general anesthesia. This medicine allows you to sleep through the surgery. A tube may be put into your throat to help you breathe.
-
You may have an epidural to help control post-surgery pain. A small tube is inserted into your back to deliver pain medicine that numbs the lower body. Talk with your healthcare provider, anesthesiologist, or nurse anesthetist about this option.
During the surgery:
-
A cut (incision) is made in the lower belly.
-
The lymph nodes near the bladder may be removed. These are checked for cancer cells (a sign that cancer has spread).
-
During simple cystectomy, the bladder is removed. During radical cystectomy, some nearby organs, such as the prostate and seminal vesicles, may also be removed. If possible, nerves that affect sexual function are not removed.
-
For a neobladder, a piece of the small intestine is removed. It is linked to the ureters on one end and to the urethra on the other.
-
For a pouch, the end of the small intestine and first part of the large intestine is removed. A stoma is made in the wall of your lower belly. The piece of intestine is then connected to the ureters on one end and to the stoma on the other.
-
Thin tubes (stents) may be placed through the belly into the ureters to the kidneys. These help drain urine during healing.
-
If you have a neobladder, a catheter may be placed into it to help drain urine. If you have a pouch, a catheter may be placed through the stoma into the pouch to keep the pathway open. Another catheter may be placed through the belly into the pouch to help drain mucus and urine.
-
Once surgery is done, the belly incision is closed with stitches (sutures) or staples. A tube (drain) may be placed to drain extra fluid from the surgical area.
Recovering in the hospital
After the surgery, you will be taken to the post anesthesia care unit (PACU) where you will be closely monitored as you wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. When you are awake and stable, you will be taken to your hospital room. While in the hospital:
-
You will be given medicine to manage pain. Let your providers know if your pain is not controlled.
-
You’ll first receive IV fluids only. In a day or so, you will start on a liquid diet. You will then slowly return to a normal diet.
-
As soon as you’re able, you will get up and walk.
-
You’ll be taught coughing and breathing methods to help keep your lungs clear and prevent pneumonia.
-
A healthcare provider will show you how to care for your neobladder or pouch and stoma. You’ll also learn how to care for any drains and tubes that you have. You may be taught to flush your pouch with fluid to remove mucus.
Recovering at home
After your hospital stay, you will be released to an adult family member or friend. Have someone stay with you for the next few days to help care for you. Recovery time varies for each person. Your healthcare provider will tell you when you can return to your normal routine. Until then, follow the instructions you have been given. Make sure to:
-
Take all medicines as directed.
-
Care for your incision as instructed. If you went home with drains or catheters, care for these as you were shown.
-
If you have a stoma, care for it as instructed.
-
Follow your healthcare provider’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that will cover the incision with water until your provider says it’s OK.
-
Don't lift anything heavy or do strenuous activities, as directed.
-
Don't drive until your provider says it’s OK. Don't drive if you’re taking medicines that make you drowsy or sleepy.
-
Walk a few times daily. As you feel able, slowly increase your pace and distance.
-
Don't strain to pass stool. If needed, take stool softeners as advised by your provider.
-
Do pelvic floor (Kegel) exercises as instructed.
When to call the healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Fever of 100.4° F ( 38°C ) or higher, or as directed by your provider
-
Symptoms of infection at an incision site, such as increased redness or swelling, warmth, worsening pain, or bad-smelling drainage
-
Pain, redness, swelling, odor, or drainage at the stoma site
-
Little or no urine output for longer than 4 hours
-
Burning or pain when passing urine or needing to pass urine often
-
Bloody urine with clots
-
Leg pain or swelling
-
Nausea or vomiting that doesn’t go away
-
Pain that can't be controlled with medicines
-
Problems with any drains, stents, or catheters
Call 911
Call 911 right away if you have:
Follow-up care
You will have follow-up visits so your healthcare provider can check how well you’re healing. Stitches, staples, or tubes will be removed. You may be taught how to drain your pouch using a catheter. If you have a neobladder, you may be taught pelvic floor exercises to strengthen the muscles around it. This helps prevent urine leakage. You and your provider can also talk about any further treatment you may need.
Risks and possible complications
All procedures have risks. Some possible risks of this procedure include:
-
Bleeding (may require a blood transfusion)
-
Infection
-
Blood clots
-
Pneumonia or other lung problems
-
Abnormal levels of vitamins and minerals in the blood, requiring lifelong medicine
-
Cancer recurrence or failure to remove all of the cancer
-
Problems with the neobladder or stoma
-
Scarring and narrowing of the ureters
-
Incontinence (unable to control urine)
-
Bowel blockage
-
Problems with sexual function or with fertility
-
Risks of anesthesia (the anesthesiologist or nurse anesthetist will talk about these with you)